Serious Psychological Distress and Mortality among Adults in the U.S. Household Population: Highlights
|
Mental illness, one of the major public health issues in the United States, has been associated with an increased risk of mortality.1 Reducing this association is part of a larger public health goal to increase life expectancy. To that end, organizations such as the Substance Abuse and Mental Health Services Administration (SAMHSA) and the National Association of State Mental Health Program Directors (NASMHPD) have indicated that monitoring premature mortality attributable to mental illness is crucial for understanding factors that affect this population in order to identify strategies that can improve the lives of people with mental illness.2,3
This issue of The CBHSQ Report presents findings extracted from a more comprehensive report on the association between one measure of mental illness (psychological distress) and mortality. The larger report provides more detailed information on the analytic techniques and death indices examined, as well as additional findings. The comprehensive report is available at https://www.samhsa.gov/data/2K14/NSDUHDR/NSDUH-DR-mental-disorders-2014.htm. Data used in both reports are from public use files for the 1997 to 2004 National Health Interview Survey (NHIS), which are linked to death certificate data from the 1997 to 2006 National Death Index (NDI).4 The analysis is based on a sample of 238,811 adults, of whom 16,568 were identified as having died during the period between the NHIS interview and December 31, 2006.
Serious Psychological Distress
Past month psychological distress was measured in the NHIS using the Kessler-6 (K6) scale.5 The K6 measures psychological distress with six questions (e.g., "how often did you feel nervous?" "how often did you feel hopeless?") scored on a five-point Likert scale, ranging from "none of the time" to "all of the time." Respondents with a score of 13 or greater on the K6 scale are identified as having serious psychological distress (SPD). An annual average of 3.1 percent of adults (6 million persons) had past month SPD at baseline (i.e., time at which they completed the NHIS survey). Adults with SPD were more likely than adults without SPD to be aged 45 to 54 years, be female, have less than a high school education, not be covered by insurance, be obese, be current smokers, use assistive living devices, and have been told by a doctor that they had heart disease, stroke, cancer, lung disease, diabetes, or hypertension (data not shown).
Serious Psychological Distress and Death Rate
Among adults aged 18 or older, the death rate increased with increasing age overall.6 The age-adjusted death rate for this age range was 865 per 100,000 person-years,7 and the rate was more than twice as high among those with SPD than among those without SPD (1,763 vs. 840 per 100,000 person-years) (Figure 1). Furthermore, adults with SPD had significantly higher age-adjusted death rates for each of the three leading causes of death (heart disease, cancer/malignant tumors, and assaults/accidents/unintentional poisonings) compared with those without SPD.
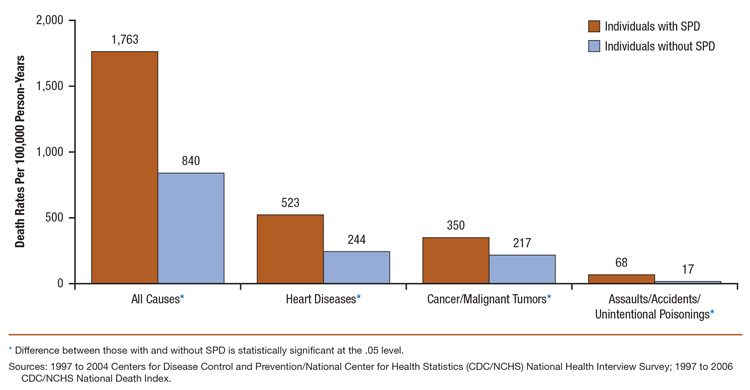 |
| Death Rates per 100,000 Person-Years |
All Causes* | Heart Diseases* | Cancer/Malignant Tumors* |
Assaults/Accidents/ Unintentional Poisonings* |
|---|---|---|---|---|
| Individuals with SPD | 1,763 | 523 | 350 | 68 |
| Individuals without SPD | 840 | 244 | 217 | 17 |
| * Difference between those with and without SPD is statistically significant at the .05 level. Sources: 1997 to 2004 Centers for Disease Control and Prevention/National Center for Health Statistics (CDC/NCHS) National Health Interview Survey; 1997 to 2006 CDC/NCHS National Death Index. |
Serious Psychological Distress and Risk of Death
Unadjusted comparisons suggest that adults with SPD were about 1.84 to 3.53 times more likely than those without SPD to have died during the follow-up period in the three age groups examined (Figure 2). After adjusting for gender, race/ethnicity, education, marital status, chronic health conditions, smoking, and obesity, the magnitude of these risks attributed to SPD was reduced but remained significant in each age group.
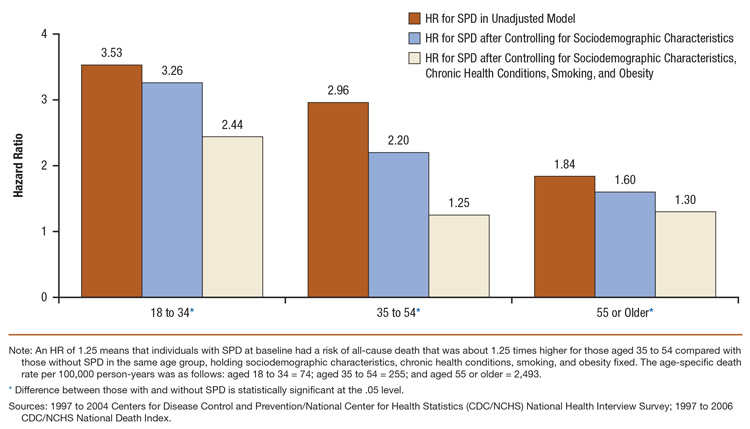 |
| Hazard Ratio | 18 to 34* | 35 to 54* | 55 or Older* |
|---|---|---|---|
| HR for SPD in Unadjusted Model | 3.53 | 2.96 | 1.84 |
| HR for SPD after Controlling for Sociodemographic Characteristics | 3.26 | 2.20 | 1.60 |
| HR for SPD after Controlling for Sociodemographic Characteristics, Chronic Health Conditions, Smoking, and Obesity |
2.44 | 1.25 | 1.30 |
| Note: An HR of 1.25 means that individuals with SPD at baseline had a risk of all-cause death that was about 1.25 times higher for those aged 35 to 54 compared with those without SPD in the same age group, holding sociodemographic characteristics, chronic health conditions, smoking, and obesity fixed. The age-specific death rate per 100,000 person-years was as follows: aged 18 to 34 = 74; aged 35 to 54 = 255; and aged 55 or older = 2,493. * Difference between those with and without SPD is statistically significant at the .05 level. Sources: 1997 to 2004 Centers for Disease Control and Prevention/National Center for Health Statistics (CDC/NCHS) National Health Interview Survey; 1997 to 2006 CDC/NCHS National Death Index. |
Years of Potential Life Lost
The measure of average years of potential life lost (YPLL) was used to compare the burden of premature mortality between individuals with and without psychological distress.8 The average YPLL is an estimate of the average years a person would have lived had he or she not died prematurely.
Adults aged 18 or older who had SPD at baseline and died during the follow-up period lost an average YPLL of 17.9. Those who did not have SPD and died lost an average YPLL of 14.1 (Figure 3). Thus, there was an additional 3.8 average YPLL for persons with SPD who died compared with those without SPD who died.
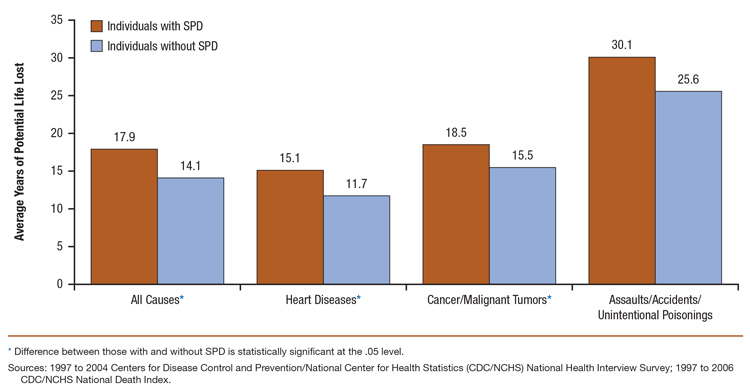 |
| Estimated Average Years of Potential Life Lost |
All Causes* | Heart Diseases* | Cancer/Malignant Tumors* |
Assaults/Accidents/ Unintentional Poisonings |
|---|---|---|---|---|
| Individuals with SPD | 17.9 | 15.1 | 18.5 | 30.1 |
| Individuals without SPD | 14.1 | 11.7 | 15.5 | 25.6 |
| * Difference between those with and without SPD is statistically significant at the .05 level. Sources: 1997 to 2004 Centers for Disease Control and Prevention/National Center for Health Statistics (CDC/NCHS) National Health Interview Survey; 1997 to 2006 CDC/NCHS National Death Index. |
Adults with SPD who died of heart diseases or cancer/malignant tumors during the follow-up lost an average of 3.4 and 3.0 more years of potential life, respectively, than those without SPD who died from heart diseases or cancer/malignant tumors. There appears to be a large difference by SPD status in the average YPLL (4.5 years) for deaths from assaults/accidents/unintentional poisonings; however, this difference did not reach statistical significance.
Discussion
Mental illness contributes to premature death in the U.S. household population. Results from this study show a robust association between one measure of mental illness (i.e., SPD) and death, even after adjusting for sociodemographic risk factors, smoking, obesity, and chronic health conditions.
The reduced life expectancy of persons with SPD underscores the importance of efforts to lessen the burden associated with mental illness. The higher rates of smoking and chronic health conditions among those with SPD suggest that the integration of primary and behavioral health care may work toward reducing the mortality gap between persons with and without SPD.
End Notes
1 Parks, J., Svendsen, D., Singer, P., Foti, M. E., & Mauer, B. (2006). Morbidity and mortality in people with serious mental illness. Alexandria, VA: National Association of State Mental Health Program Directors (NASMHPD) Medical Directors Council.
2 Center for Mental Health Services. (2011). About SAMHSA's wellness efforts. Retrieved from http://www.promoteacceptance.samhsa.gov/10by10/default.aspx
3 Lutterman, T., Ganju, V., Schacht, L., Shaw, R., Monihan, K., & Huddle, M. (2003). Sixteen state study on mental health performance measures (HHS Publication No. SMA 03-3835). Retrieved from http://www.nri-inc.org/reports_pubs/2003/16StateStudy2003.pdf
4 Centers for Disease Control and Prevention. (2012, May 2). National Health Interview Survey: Home page. Retrieved from http://www.cdc.gov/nchs/nhis.htm
5 Kessler, R. C., Barker, P. R., Colpe, L. J., Epstein, J. F., Gfroerer, J. C., Hiripi, E., Hiripi, E., Howes, M. J., Normand, S. L., Manderscheid, R. W., Walters, E. E., & Zaslavsky, A. M. (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60, 184-189.
6 The age-specific death rate per 100,000 person-years was as follows: aged 18 to 34 = 74; aged 35 to 44 = 154; aged 45 to 54 = 362; aged 55 to 64 = 802; aged 65 to 74 = 1,930; and aged 75 or older = 5,862.
7 Interpretations of the death rates presented should be made with caution because these rates were age adjusted only and did not control for other characteristics.
8 The calculation for this measure involved those study respondents who died during the follow-up period. YPLL were calculated by multiplying the number of deaths at each age with the reference sex-specific life expectancy at that age, and the quantities were then summed across all ages at death to get the total YPLL. The total YPLL were divided by the total number of deaths to get the average YPLL per decedent.
Suggested Citation
Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (August 7, 2014). The CBHSQ Report: Serious Psychological Distress and Mortality among Adults in the U.S. Household Population: Highlights. Rockville, MD.
| The Substance Abuse and Mental Health Services Administration (SAMHSA) is the agency within the U.S. Department of Health and Human Services that leads public health efforts to advance the behavioral health of the nation. SAMHSA's mission is to reduce the impact of substance abuse and mental illness on America's communities. |
CBHSQ_160